As a gut health dietitian, I’ve seen soooo many patients struggling with weird stomach problems only to discover they’re hosting an uninvited guest: Helicobacter pylori.
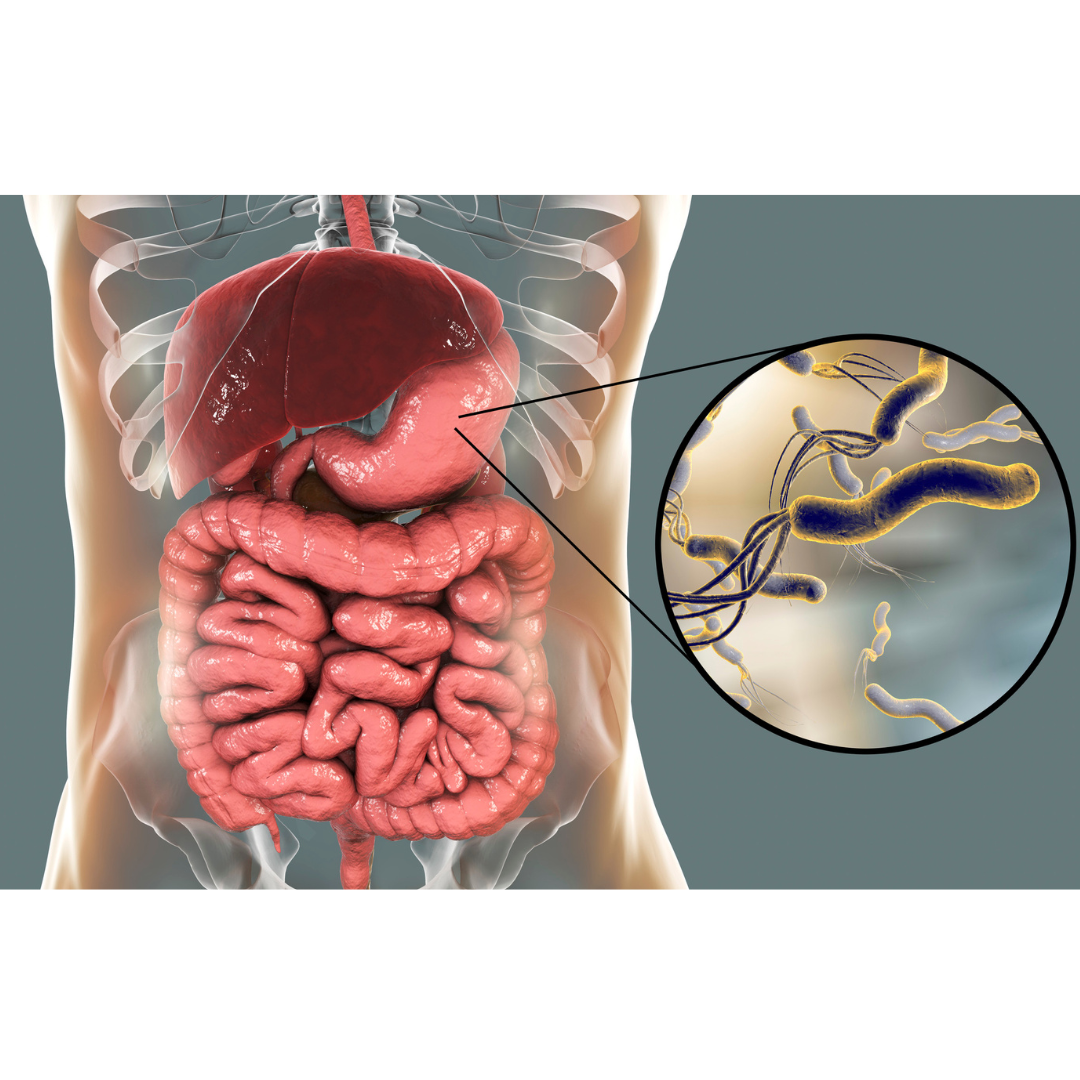
This corkscrew-shaped bacteria affects nearly half the world’s population and can be particularly troublesome if left untreated.
But don’t worry—understanding H. pylori and knowing how to manage it through diet can make a world of difference in your digestive health journey.
What Exactly Is H. pylori?
H. pylori is a sneaky little bacteria that has evolved to survive in the harsh, acidic environment of your stomach.
Think of it as that annoying houseguest who shows up uninvited and then refuses to leave—except instead of eating all your snacks, it damages your stomach lining!
This bacterial infection is known for causing:
- Gastritis (inflammation of the stomach lining)
- Peptic ulcers
- Reflux or GERD
- In some cases, increasing the risk of stomach cancer
- Various digestive symptoms including bloating, nausea, and abdominal pain
Causes of H. pylori Infection in Adults
The exact transmission routes of H. pylori aren’t fully understood, but several pathways have been identified:
Person-to-Person Contact
The most common transmission route is through close personal contact. That’s right—H. pylori can spread through:
- Saliva (kissing or sharing utensils or food)
- Oral-oral transmission
- Fecal-oral routes (due to poor hand washing techniques)
Think twice before sharing that spoon with someone who has all the GI symptoms! Even your own flesh and blood.
Contaminated Food and Water
This is particularly common in regions with poor sanitation, but is actually a common cause in Western societies as well:
- Consuming food prepared by someone with poor hand hygiene
- Drinking water from contaminated sources
- Eating raw or undercooked food that hasn’t been properly washed
Environmental Factors
Some research suggests H. pylori may persist in:
- Soil in certain regions
- Water systems
- Food growing environments
Occupational Risk
Healthcare workers and gastroenterologists may have higher exposure rates due to:
- Performing endoscopic procedures
- Handling specimens containing the bacteria
Causes of H. pylori Infection in Children
Children are particularly vulnerable to H. pylori infection, and the acquisition patterns differ slightly from adults:
Family Transmission
The most significant risk factor for children is living with family members who have H. pylori:
- Parent-to-child transmission (especially mother-to-child)
- Sharing beds, utensils, or food with infected family members
- Poor household hygiene practices
Daycare and School Settings
Children in group settings may be at higher risk due to:
- Close contact with other children
- Less vigilant hand-washing habits
- Sharing of toys and other items that may be contaminated
Early Life Acquisition
Many people actually acquire H. pylori before age 5, and then carry it into adulthood without symptoms until later in life.
That’s right! H. pylori can live in your body for years (and years) if it’s not eliminated.
Crowded Living Conditions
Children living in crowded homes with limited access to clean water and proper sanitation are at higher risk of infection.
H. pylori is super common in college and university students… they not only share food, drinks, and utensils, but they also have lots friends coming and going from their rooms or houses. My youngest son tested positive for H. pylori (and he had all the symptoms) after moving to a house inhabited by a bunch of dudes. If you’re a parent of a boy… you understand the issue. Girls have the same problem, even though they tend to be less piggy.
Signs You Might Be Hosting This Unwelcome Guest
H. pylori doesn’t always announce its presence with symptoms, which is partly why it’s so successful at colonizing in humans and why we always test for this little guy. (Get info on why we’re so successful at clearing H. pylori with comprehensive gut testing here.) However, common signs include:
- Gnawing or burning stomach pain (especially when your stomach is empty)
- Nausea or vomiting
- Reflux
- Frequent burping
- Bloating sensation
- Lack of appetite or feeling full with small meal
- Unintended weight loss or gain
- Bad breath that brushing doesn’t seem to fix
In children, symptoms may also include:
- Recurrent abdominal pain
- Iron-deficiency anemia
- Growth issues
- Recurrent vomiting
Remember: many people with H. pylori have no symptoms at all! That’s why it can go undetected for years or even decades.
Dietary Strategies to Support H. pylori Treatment
While antibiotics are the primary treatment for H. pylori, certain dietary approaches can support the treatment process and help manage symptoms. Here’s what to focus on:
Foods to Embrace
1. Probiotics Powerhouses
Research suggests probiotics may help improve H. pylori eradication rates when used alongside antibiotics:
- Yogurt with live cultures (look for those that contain Lactobacillus and Bifidobacterium strains) – choose dairy-free options if you can’t tolerate the dairy. We love Cocojune!)
- Kefir
- Fermented vegetables like unpickled sauerkraut and kimchi (check out Bubbie’s brand)
2. Antioxidant-Rich Foods
These foods help fight inflammation and support healing:
- Colorful berries (blueberries, strawberries, blackberries)
- Leafy greens (spinach, kale, arugula)
- Orange and yellow vegetables (carrots, sweet potatoes, bell peppers)
- Cruciferous vegetables (broccoli, cauliflower, cabbage, Brussels sprouts)
3. Prebiotic Foods
These foods feed your beneficial gut bacteria:
- Garlic and onions (in moderate amounts, if tolerated)
- Bananas (especially slightly underripe ones)
- Apples
- Rice (we love black rice!)
- Jerusalem artichokes, aka sunchokes
- Asparagus
But the truth is that most plant-based foods contain some level of prebiotics. Eat what you enjoy!
4. Anti-Inflammatory Foods
These foods help reduce stomach inflammation:
- Fatty fish rich in omega-3s (salmon, mackerel, sardines) – fresh, not smoked or salt-preserved
- Extra virgin olive oil (especially that with high polyphenol count)
- Seeds like flax, sunflower, and pumpkin seeds
- Walnuts and other tree nuts (except almonds)
- Turmeric with black pepper
- Ginger (check out cauli rice recipe here and fermented ginger applesauce recipe here)
5. Green Tea
Some studies suggest that green tea may have antimicrobial properties that could help fight H. pylori.
Foods That May Irritate Your Stomach
1. Acidic Foods
These can irritate an already sensitive stomach lining:
- Citrus fruits and juices
- Tomatoes and tomato-based products
- Vinegar and vinegar-containing foods
- Coffee and tea (except green tea)
2. Spicy Foods
Chili peppers, hot sauces, and heavily spiced dishes may aggravate symptoms.
3. Alcohol
Alcohol can irritate the stomach lining and potentially interact with antibiotics if you’re on treatment.
4. Processed Foods
These typically contain preservatives and additives that may irritate your stomach:
- Fast food
- Packaged snacks
- Processed meats
- Frozen meals with many ingredients
5. Sugar and Refined Carbohydrates
These can feed harmful bacteria and promote inflammation:
- Sugary desserts and candies
- White bread, pasta, and rice
- Sweetened beverages
6. Common Irritants and Allergens
These foods may trigger symptoms in many people with H. pylori and can help it multiply:
- Chocolate and cocoa products
- Oats
- Almonds and almond products
- Soy and soy-based foods
- Smoked foods (including smoked meats and fish)
- Pickled foods
- Salt-preserved foods
- Fresh and dried legumes (including beans, lentils, chickpeas, and peas)
Why Certain Foods Can Be Problematic with H. pylori
When managing H. pylori infection, understanding why certain foods may worsen symptoms can help you make informed dietary choices.
And besides worsening symptoms, these foods have been shown to feed H. pylori so that it can grow and thrive. Let’s explore why the foods we’ve recommended avoiding might cause digestive issues:
Chocolate and Cocoa
Chocolate contains several compounds that can be troublesome for those with H. pylori:
- Caffeine can increase stomach acid production
- Theobromine may relax the lower esophageal sphincter, potentially worsening reflux symptoms
- Fat content in chocolate can slow digestion and exacerbate symptoms
- Sugar can feed unwanted bacteria in the gut
Oats
While generally considered healthy, oats may be problematic because:
- Their high fiber content can be difficult to digest when the stomach lining is inflamed
- They contain avenin, a protein that some people react to similarly to gluten
- Phytic acid in oats may bind to minerals and make existing nutritional deficiencies worse
- The fermentation of oats in the gut may increase gas production and bloating
Almonds
Despite their health benefits for many, almonds might aggravate H. pylori symptoms due to:
- Their hard texture, which requires more stomach acid to digest
- Enzyme inhibitors that can interfere with digestion
- High fat content that may slow gastric emptying
- Potential allergenic properties that could add to inflammation
Soy and Soy Products
Soy can be problematic because:
- It contains phytoestrogens that may affect hormonal balance and potentially interact with H. pylori
- Enzyme inhibitors in soy can interfere with protein digestion
- Phytic acid content can bind to minerals like zinc, which is important for healing the gut lining
- Many people have sensitivities to soy proteins that can increase inflammation
Smoked, Pickled, and Salt-Preserved Foods
These preservation methods create compounds that can be harmful:
- High salt content can irritate the stomach lining and potentially support H. pylori survival
- Nitrates and nitrites in cured meats have been associated with increased gastric cancer risk
- Polycyclic aromatic hydrocarbons in smoked foods may be carcinogenic
- High acidity in pickled foods can irritate an already inflamed stomach
Fresh and Dried Legumes
Legumes might cause issues because:
- They contain oligosaccharides (FODMAPS) that can ferment in the gut, causing gas and bloating
- Lectins and phytates can interfere with nutrient absorption and digestion
- Their high fiber content may be difficult to digest during active infection
- Complex proteins in legumes can be challenging to break down when digestive function is compromised
General Recommendations
Remember that food sensitivities are highly individual. What triggers symptoms in one person with H. pylori may be perfectly tolerable for another. This is why keeping a food journal is so valuable—it helps you identify your personal trigger foods.
As your gut heals following H. pylori treatment, you may find that you can gradually reintroduce some of these foods. Start with small amounts and monitor how you feel. The goal isn’t to restrict your diet forever, but rather to support healing during the acute phase of infection and treatment.
A Week of H. pylori-Friendly Meals
Here’s a sample meal plan that incorporates H. pylori-friendly foods while avoiding common irritants and the specified exclusions (chocolate/cocoa, oats, almonds, soy, smoked/pickled/salt-preserved foods, fresh and dried legumes):
Monday
Breakfast: Quinoa breakfast bowl with sliced banana, a sprinkle of ground flaxseed, and a dollop of plain probiotic yogurt (choose dairy-free if needed)
Lunch: Bowl with arugula, steamed broccoli, carrots, and grilled chicken, drizzled with olive oil and gentle herbs like oregano, basil, or mint
Dinner: Baked salmon with a side of mashed sweet potato (recipe here) and steamed asparagus
Snack: Fresh blueberries with a small cup of coconut yogurt
Tuesday
Breakfast: Smoothie with coconut kefir, spinach, banana, and a tablespoon of sunflower seed butter
Lunch: Ground turkey and avocado wrap with shredded carrots in a butter lettuce “tortilla”
Dinner: Herbed chicken soup with carrots, celery, and mild herbs (no onions if sensitive)
Snack: Apple slices with a thin spread of sunflower seed butter
Wednesday
Breakfast: Two scrambled eggs with spinach and a side of sliced melon
Lunch: Baked sweet potato topped with arugula, pickled onions, pumpkin seeds, diced grilled chicken, and diced avocado
Dinner: Grilled beef tenderloin with roasted Brussels sprouts and a few tablespoons of fermented sauerkraut
Snack: Plain yogurt with a drizzle of honey and sliced strawberries
Thursday
Breakfast: Chia pudding made with coconut milk, topped with blueberries and a sprinkle of cinnamon
Lunch: Mediterranean salad with cucumbers, bell peppers, kalamata olives, fresh oregano and basil, red onion, and grilled chicken (skip the tomatoes if sensitive)
Dinner: Baked cod with a side of steamed green beans and black (forbidden) rice
Snack: A small handful of pumpkin seeds and a crisp pear
Friday
Breakfast: Rice porridge (congee) topped with sliced apple, cinnamon, and a dollop of yogurt (dairy-free if sensitive to dairy)
Lunch: Chicken and vegetable soup with carrots, celery, and brown rice (mild herbs, no onions if sensitive)
Dinner: Grilled zucchini and bell peppers with herbed quinoa and baked salmon
Snack: Cucumber slices and snap peas with guacamole
Saturday
Breakfast: Yogurt parfait with layers of fresh berries (add a scoop of protein powder, if desired)
Lunch: Tuna salad (or sub out sardines) (made with olive oil instead of mayo) on a bed of mixed greens
Dinner: Baked chicken thighs with roasted root vegetables and quinoa
Snack: A small bunch of grapes and a few cubes of cheese
Sunday
Breakfast: Whole grain toast (gluten-free) topped with smashed avocado and a poached egg
Lunch: Warm grain bowl with black rice, roasted butternut squash, spinach, avocado, pumpkin seeds, fermented onions, and grilled chicken
Dinner: Mild vegetable curry with diced chicken served over brown rice
Snack: Kefir smoothie with banana
Tips for Success
- Eat smaller, more frequent meals rather than three large ones to reduce pressure on your stomach.
- Stay hydrated with water and herbal teas like chamomile or ginger.
- Chew food thoroughly to aid digestion and reduce stress on your stomach.
- Keep a food journal to identify personal trigger foods that may exacerbate symptoms.
- Don’t eat right before bed – try to have your last meal at least 3 hours before sleeping.
- Consider supplements like zinc carnosine, mastic gum, or DGL licorice – but always consult with your healthcare provider first.
Prevention: Keeping H. pylori Away
Whether you’re trying to prevent first-time infection or reinfection after treatment, these practices are essential:
Hygiene Practices
- Wash hands thoroughly before eating and after using the bathroom
- Avoid sharing utensils, cups, or toothbrushes
- Use clean water for drinking and food preparation
Food Safety
- Thoroughly cook all animal products
- Wash fruits and vegetables carefully
- Be cautious when eating out, especially in regions with poor sanitation
For Children
- Teach proper hand hygiene early
- Avoid mouth-to-mouth feeding practices
- Ensure clean drinking water and food at school or daycare
When to See a Healthcare Practitioner
While dietary changes can help manage symptoms and support treatment, they’re not a substitute for medical care. Consult your healthcare practitioner if you experience:
- Persistent abdominal pain
- Black or bloody stools
- Severe or persistent heartburn
- Unexplained weight loss
- Difficulty swallowing
- Persistent vomiting
Remember, H. pylori requires proper medical diagnosis (We are experts at this!) and treatment for eradication. Once treatment has been successful, it is crucial to get the gut “environment” optimized so that you are less likely to be reinfected with H. pylori. The dietary strategies discussed here are complementary approaches, not treatments.
The Takeaway: H. pylori Isn’t Forever
Living with H. pylori doesn’t have to mean living with constant discomfort. By combining proper medical treatment with these dietary strategies, you can show this unwelcome stomach guest the door and restore your digestive health.
Your stomach has been H. pylori’s host long enough—it’s time to kick it to the curb and say hello to better gut health!
Gut Health Diagnosis at EverVital Nutrition
Are you struggling with chronic gut symptoms and you suspect an H. pylori infection? We can help!
At EverVital Nutrition, we use specific diagnostic tools to determine your level of gastrointestinal overgrowth (which is very common with patients taking GLP-1 meds, antibiotics, or antihistamines), digestive function, and inflammation. It’s a comprehensive gut microbiome test, rather than a guess.
To learn more about gut testing and get on the path to healing so you can live the life you want without symptoms, scan the QR code below to schedule your free gut assessment!